If you or a loved one has recently been diagnosed with PKAN, we hope our website can help answer some of your questions and guide you to the most appropriate resources. We encourage you to call our team to speak to a genetic counselor who can help you navigate this diagnosis. Please email us at info@nbiacure.org and we will set up a phone call with you.
PKAN (Pantothenate Kinase-Associated Neurodegeneration) is one of the most common NBIA disorders. Based on the age of onset and rate of progression, individuals with PKAN may be classified as having classic or atypical forms. However, as we learn more about PKAN, we have found that some people fall between these 2 categories. In other words, there is a broad spectrum of symptoms.
SYMPTOMS
The symptoms of atypical PKAN are more variable than those of classic PKAN and appear at a later age. A person with atypical PKAN will begin to show symptoms before they reach their 30s, on average around age 13.
Common symptoms include:
Speech problems (commonly the first noticed symptom)
- Palilalia (repetition of words or phrases)
- Achylalia/tachylogia (rapid speech of words and/or phrases)
- Dysarthria (poor articulation or slurring)
- All of these progressive speech problems can make it difficult to be understood by acquaintances and others in the community. Usually people close to the individual with PKAN have learned to better understand their speech
Psychiatric symptoms
- Personality changes with impulsivity or outbursts
- Depression
- Emotional lability (unpredictable changes in emotions)
- Motor and verbal tics
- Obsessive-compulsive behavior
- Rarely some psychotic symptoms
Cognitive changes
- Atypical PKAN causes fewer intellectual and behavior changes than classic PKAN
- More research is needed to determine the extent of impairment
Motor involvement (usually develops later in life)
- Spasticity (stiff muscles)
- Dystonia (involuntarily muscle contraction and spasms)
- Parkinsonism (symptoms similar to Parkinson’s disease):
- Tremors (shaking)
- Hypokinesia (decreased muscle movement)
- Rigidity (stiffness)
- Postural instability (loss of balance that causes unsteadiness)
- Hyperreflexia (overactive reflexes)
- Other signs of corticospinal tract (communication pathway between brain and limbs) involvement
Other features associated with atypical PKAN, such as essential tremor-like syndrome and retinopathy, are rare.
CAUSE/GENETICS
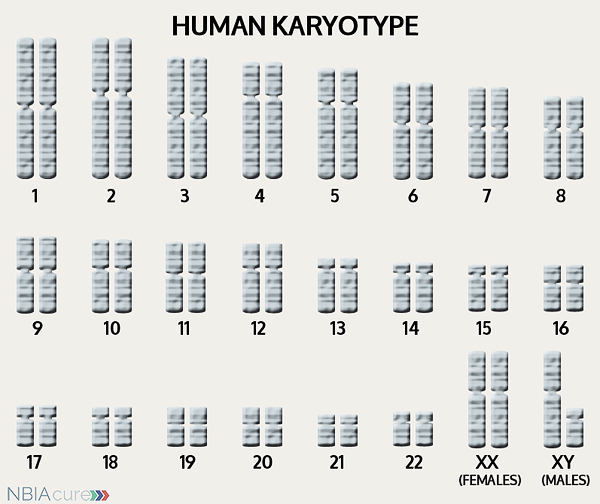 The human body is made up of millions of cells. Inside every cell there is a structure called DNA, which is like an instruction book. DNA contains detailed steps about how all the parts of the body are put together and how they work. However, DNA contains too much information to fit into a single “book,” so it is packaged into multiple volumes called chromosomes. Humans typically have 46 total chromosomes that are organized in 23 pairs. There are two copies of each chromosome because we receive one set of 23 chromosomes from our biological mother and the other set of 23 from our biological father. Chromosomes 1-22 are called autosomes and the last pair is called the sex chromosomes because they determine a person’s gender. Females have two X chromosomes and males have one X and one Y.
The human body is made up of millions of cells. Inside every cell there is a structure called DNA, which is like an instruction book. DNA contains detailed steps about how all the parts of the body are put together and how they work. However, DNA contains too much information to fit into a single “book,” so it is packaged into multiple volumes called chromosomes. Humans typically have 46 total chromosomes that are organized in 23 pairs. There are two copies of each chromosome because we receive one set of 23 chromosomes from our biological mother and the other set of 23 from our biological father. Chromosomes 1-22 are called autosomes and the last pair is called the sex chromosomes because they determine a person’s gender. Females have two X chromosomes and males have one X and one Y.
If DNA is the body’s instruction book and it is stored in multiple volumes (called chromosomes), then genes would be the individual chapters of those books. Genes are small pieces of DNA that regulate certain parts or functions of the body. Sometimes multiple genes (or chapters) are needed to control one function. Other times, just one gene (or chapter) can influence multiple functions. Since there are two copies of each chromosome, there are also two copies of each gene. In some gene pairs, both copies need to be expressed (or turned on) in order for them to do their job correctly. For other genes pairs, only one copy needs to be expressed.
When a single cell in the human body divides and replicates, its DNA is also replicated. This replication process is usually very accurate but sometimes the body can make a mistake and create a “typo” (or gene change). Just like a typo in a book, a gene change in the DNA can be unnoticeable, harmless, or serious. A gene change with serious consequences can result in a part of the body not developing correctly or a particular function not working properly.
In the case of NBIA disorders, changes in certain genes cause a person to develop a particular type of NBIA. PANK2 is the only gene known to cause PKAN. PANK2’s main job is to tell the body’s cells how to turn vitamin B5 (pantothenate) into an essential chemical (coenzyme A). Coenzyme A plays a key role in the body’s energy metabolism. It is not yet clear to us how the decrease in coenzyme A eventually leads to iron accumulation in the brain.
In contrast to individuals with classic PKAN, those with atypical PKAN are more likely to have PANK2 gene changes that allow some iron to be metabolized (broken down) so there is less iron accumulation in the brain.
As mentioned earlier, humans have a total of 23 pairs of chromosomes. Half of these chromosomes are passed down (or inherited) from the biological mother and half from the biological father. The way in which a gene carrying a change is passed down from parents to child varies from gene to gene. The PANK2 gene that is mutated in those with PKAN is inherited in an autosomal recessive manner.
“Autosomal” refers to the fact that the PANK2 gene is located on chromosome 20, which is one of the autosomes (chromosome pairs 1-22). Since the sex chromosomes are not involved, males and females are equally likely to inherit a gene change located in the autosomes. “Recessive” refers to the fact that a gene change must be present in both copies of the PANK2 gene for a person to have PKAN. If an individual has only one PANK2 gene change, then they are called a “carrier” for PKAN. Carriers do not have health problems related to the gene change and often do not know they carry a recessive gene change. However, if two PKAN carriers have a child together, then there is a 25% chance that they will both pass on their recessive PANK2 gene changes and have a child with PKAN.
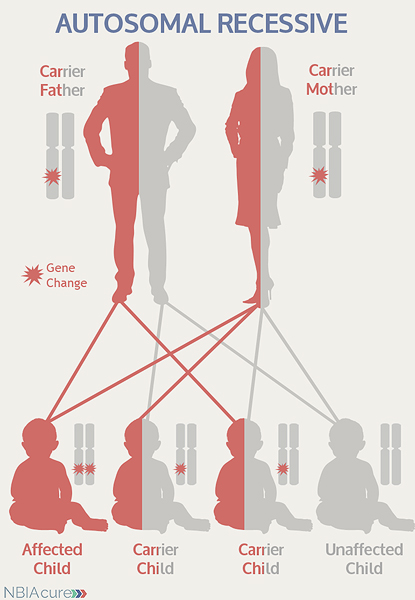 As seen in the image to the left, in a pregnancy between two PKAN carriers:
As seen in the image to the left, in a pregnancy between two PKAN carriers:
- There is a 25% chance of the child having PKAN
- There is a 50% chance that the child will be a carrier like his/her parents
- There is a 25% chance that the child will not have PKAN or be a carrier
DIAGNOSIS & TESTING
A brain MRI is a standard diagnostic tool for all NBIA disorders. MRI stands for magnetic resonance imaging. An MRI produces a picture of the body that is created using a magnetic field and a computer. The technology used in an MRI is different from that of an x-ray. An MRI is painless and is even considered safe to do during pregnancy. Sometimes an MRI is done of the whole body, but more often, a doctor will order an MRI of one particular part of the body.
Evidence of iron accumulation on a brain MRI is often an important clue leading to the diagnosis of PKAN. A T2 sequence is the preferred type of MRI for NBIA diagnosis because it is highly sensitive to the detection of brain iron.
In both the classic and atypical forms of PKAN, an “eye of the tiger” sign is almost always seen on a brain MRI.
- Most individuals with PANK2 mutations have the “eye of the tiger” MRI sign
- Almost all individuals with the “eye of the tiger” sign have at least one PANK2 mutation
- Brain MRI has also accurately predicted PKAN in pre-symptomatic siblings of affected individuals
PKAN “Eye of the Tiger” MRI Sign
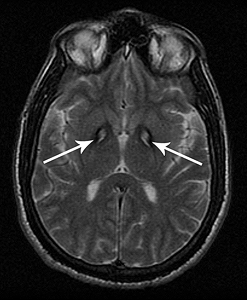 The image on the right shows a T2 MRI with an “eye of the tiger” sign. On a T2 MRI, the bright areas indicate pockets of swelling and fluid and the dark areas show iron accumulation. In the majority of PKAN cases, iron accumulation is restricted to the globus pallidus and substantia nigra regions of the brain, which help control movement.
The image on the right shows a T2 MRI with an “eye of the tiger” sign. On a T2 MRI, the bright areas indicate pockets of swelling and fluid and the dark areas show iron accumulation. In the majority of PKAN cases, iron accumulation is restricted to the globus pallidus and substantia nigra regions of the brain, which help control movement.
An “eye of the tiger” sign is defined as an area of central hyperintensity (bright) surrounded by hypointensity (dark) in the globus pallidus region of the brain. The bright areas are usually large in the first stages of PKAN and represent early damage and fluid accumulation in the tissue. The dark regions seen in the “eye of the tiger” are deposits of iron. As the disease progresses, the bright spots tend to shrink and the darker areas of iron accumulation become larger and more noticeable. The combination of a dark region with a bright center creates the “eye of the tiger” sign.
Diagnosis of PKAN is confirmed through genetic testing of the PANK2 gene to find two gene changes. At least one PANK2 gene change is found through DNA sequence analysis in greater than 99% of individuals with NBIA who had an “eye of the tiger” sign on MRI.
If no gene change or only one gene change is found through sequence analysis of the PANK2 gene, then genetic testing may proceed to deletion/duplication analysis. Among individuals who go forward with deletion/duplication analysis, a gene change will be found in approximately 3-5% of cases.
Very rarely, an individual with the signs and symptoms of PKAN will have only one or even no PANK2 gene changes identified. This can happen because genetic testing is not perfect and has certain limitations. It does not mean the person does not have PKAN; it may just mean we do not yet have the technology to find the hidden gene change. In these cases it becomes very important to have doctors experienced with PKAN review the MRI and the person’s symptoms very carefully to be as sure as possible of the diagnosis.
MANAGEMENT
 There is no standard treatment for classic PKAN. Diagnosed individuals are managed by a team of medical professionals that recommends treatments based on current symptoms.
There is no standard treatment for classic PKAN. Diagnosed individuals are managed by a team of medical professionals that recommends treatments based on current symptoms.
After diagnosis, individuals with atypical PKAN are recommended to get the following evaluations to determine the extent of their disease:
- Neurologic examination for dystonia, rigidity, and spasticity, and parkinsonism
- Evaluation of ambulation and speech
- Developmental assessment
- Assessment for physical therapy, occupational therapy, and/or speech therapy
- Medical genetics consultation
The most commonly treated atypical PKAN symptom is dystonia (involuntarily muscle contraction and spasms), which can be debilitating and distressing to affected individuals and their caregivers. The therapies for managing dystonia vary in method and success rate.
Therapies to manage dystonia can include:
- Intramuscular botulinum toxin
- Botox is injected in spastic, dystonic muscles to help them relax for a period of time
- Artane (trihexyphenidyl), taken orally, usually divided into multiple doses each day
- Baclofen (oral or intrathecal)
- One of the main drugs used to treat PKAN dystonia, usually first taken orally and divided into several doses each day
- In the intrathecal method, an implanted baclofen pump delivers medication directly into the spinal fluid
- Deep brain stimulation
- Used increasingly more often in NBIA and has some evidence for benefit
- A stimulator sends electrical impulses to the affected brain region to help muscles relax
- It involves surgical implantation of a lead, extension and battery pack (IPG)
- The lead contains 4 electrodes and is implanted in the globus pallidus region of the brain
- The extension connects the lead to the battery pack (IPG)
- The IPG is a battery-powered neurostimulator that is placed in the abdomen (or in some cases below the clavicle)
- Physical and occupational therapy
- May or may not be indicated for those who are only mildly symptomatic
- Therapies to maintain normal joint mobility for as long as possible may be useful
- Speech therapy is often indicated for PKAN-related dysarthria
Medication to manage parkinsonism:
The symptoms of parkinsonism can be treated with the same medications used in Parkinson’s disease. Treatment with Levodopa (a medication the body converts into dopamine) must be started and monitored carefully. In the beginning, the dose is increased gradually until both the patient and doctor feel symptoms are under control. While taking dopaminergic drugs, individuals must be regularly monitored for adverse neuropsychiatric effects, psychiatric symptoms and worsening of parkinsonism. Levodopa is generally not useful in the treatment of PKAN, with some rare exceptions.
Even after a diagnosis has been made and the appropriate therapies have been decided, it is recommended to continue long-term surveillance to decrease the impact of PKAN symptoms and increase quality of life.
Long-term surveillance for PKAN can include:
- Regular assessments of ambulation speech abilities
- Psychiatric treatment and monitoring
- Nutrition
- Monitoring of height and weight in children and weight in adults
- Evaluation of swallowing difficulties due to head and neck dystonia
- Oral assessment for signs of trauma
- Nutritional supplements and gastric feeding (if needed)
- Routine eye exams
- Monitoring of individuals receiving dopaminergic drugs for parkinsonism
PROGRESSION
In comparison to classic PKAN, the progression of symptoms is slower in atypical PKAN. For example, the symptoms of motor involvement develop later in life. However, like in classic PKAN, individuals with atypical PKAN cannot regain skills that they have lost.
Atypical PKAN does not progress at a consistent rate. Individuals with atypical PKAN can have episodes lasting weeks to months where they decline rapidly, followed by longer periods when they are stable. At this point in time, a reason or trigger for the periods of decline has not been found.
The average lifespan varies for individuals with atypical PKAN. Due to improvements in medical care, more affected individuals are now living well into late adulthood.
RESEARCH
You can currently enroll in (or enroll your child in) a natural history study called PKANready. The purpose of this study is to help us better understand the progression of PKAN and identify disease markers that can be used in future clinical trials. This study can be done completely from home and involves entering information every six months. You can learn more about this study and enroll here: PKANREADY
Our team, in collaboration with Dr. Sibon in the Netherlands, is developing a possible therapeutic for PKAN called CoA-Z. To learn more about the phase II clinical trial and next steps, please go here: CoA-Z Clinical Trial
HARP SYNDROME
HARP syndrome is a condition that was described in a few families prior to the discovery of the PANK2 gene. The letters H.A.R.P. refer to the main symptoms, which are also key features of PKAN:
- Hypoprebetalipoproteinemia (low levels of LDL cholesterol)
- Acanthocytosis (red blood cells shaped like spurs)
- Retinitis pigmentosa (progressive vision loss due to damage of the retina)
- Pallidal degeneration (damage in the part of the brain involved in voluntary movement)
After finding the PANK2 gene, it was recognized that HARP is a form of PKAN.
Copyright © 2014 by NBIAcure.org. All rights reserved.