When Mike Cohn was 15 years old, his unique medical history was described in the well-known medical journal, Neurology. Mike had seizures as a baby, and he reached his motor milestones later than other kids his age. When he turned 8, he felt like his world was turned upside down. Walking became increasingly difficult due to spasticity and dystonia, although he can still do it with a walker. Speech and communication became a frustrating challenge as he approached 11, and his vision worsened. Early imaging studies suggested he had abnormal iron accumulation in his brain. Eventually, Mike connected with the NBIA community and became a champion for NBIA disorders, despite not having a specific diagnosis himself. We first learned of Mike in October of 1996—just over 20 years ago. Over the years, each time a new gene was identified, we thought “maybe this one will explain Mike’s disease,” and each time it tested negative.
In medical speak, we call this a diagnostic odyssey. A journey, sometimes over decades, searching for the cause of disease. Mike’s odyssey recently reached a conclusion. During his search, he has touched thousands of people and helped stimulate a research collaboration across 4 continents. Mike’s DNA, with his permission, has traveled across the Atlantic Ocean as part of his quest. Finally, this year, just shy of his 50th birthday, Mike got an answer.
It started when our team decided to apply to the University of Washington Center for Mendelian Genomics to support a new project. Newer technologies had become available to efficiently screen thousands of genes in a single swoop. This program, if they accepted our application, would screen several of the NBIA research subjects in our repository who still lacked a specific diagnosis. Our proposal was accepted, and we got to work preparing samples and information to send 173 miles north to the University of Washington, located in Seattle.
Several months later, Washington’s Center for Mendelian Genomics had generated so much data that we had to buy a sophisticated new external hard drive just to contain it all. While an expert analyst on the Washington team started to sift through the data, we did the same in parallel at OHSU. Of the 13 individuals submitted, we were able to make new diagnoses in 7 of them based on mutations found in genes that were already known to cause diseases. Of course, Mike was one of the remaining 6 individuals who still did not have an answer. However, we did find something suspicious. Actually, 2 things.
Mike’s DNA sample showed 2 different changes in a gene called MECR. This gene encodes a protein called “mitochondrial trans-2-enoyl-CoA reductase.” Those of you who have lived with NBIA, who have delved into the complicated literature, attended family meetings, and taken your loved ones to doctor appointments, will probably notice a few interesting things about this protein: the words “mitochondrial” and “CoA” made our OHSU team giddy with excitement. The pieces of the puzzle seemed to be coming together. This gene made sense; we thought it could explain Mike’s symptoms. However, it had never been associated with human disease.
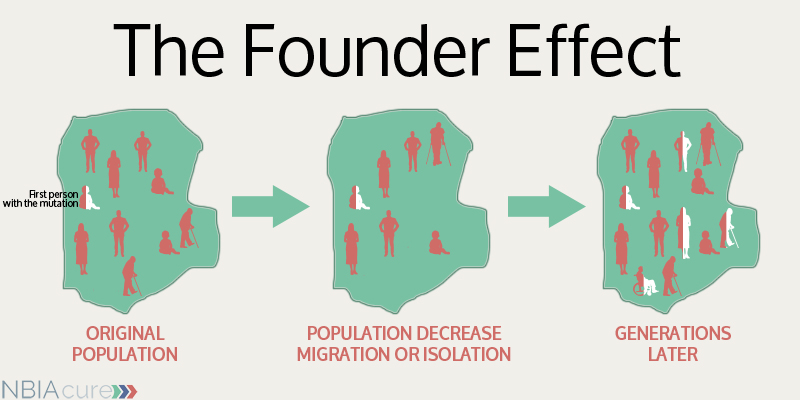
Identifying these gene mutations was a huge hurdle we had just jumped, but we still faced several more. In order to truly prove that mutations in a gene cause a certain disease, it’s necessary to find them in multiple patients with similar symptoms. In other words, we needed to build our story a little more. But Mike was one of a kind! How could we try to find others like him, when MECR wasn’t even known to cause disease? As luck would have it, there is a match-making service for genes. Sort of an eHarmony for pairing up investigators studying the same rare gene changes. It’s called GeneMatcher. With the hope of identifying another patient somewhere in the world, we created an entry in GeneMatcher and asked any investigators who found a change in MECR to contact us.
While we waited to hear back from GeneMatcher, we continued to build the story with another approach. Although MECR wasn’t known to cause human disease, a small group in Finland had been studying it as part of a biochemical pathway for several years. Dr. Hayflick reached out to investigators at the University of Oulu, Finland, to share our findings and engage their team in better understanding our discovery. They agreed to use cell models in their lab to try to prove that Mike’s gene changes would knock out the function of the MECR protein. Many months later, as the work in Finland progressed, we got exciting news: GeneMatcher had made a match! We were contacted by a physician investigator in Israel who had a patient with mutations in MECR. Even better, this patient shared a mutation in common with Mike. Although it hadn’t seemed significant until that moment, Mike happens to be of Jewish ancestry, just like the patient in Israel. Now the puzzle pieces were really coming together. As we and our collaborators continued to work and build the story, with the goal of publication, we eventually identified patients in Italy and Australia as well.
On December 1, 2016, a new paper was published in The American Journal of Human Genetics entitled “MECR mutations cause childhood-onset dystonia and optic atrophy, a mitochondrial fatty acid synthesis disorder.” Mike is the oldest individual described in the paper, although a few others are close. The youngest is only 7. Mike has a name for his medical condition now: MEPAN. It stands for a long string of complicated words: mitochondrial enoyl CoA reductase protein-associated neurodegeneration. Based on what we know about MEPAN, we even have a few ideas about potential therapies. Oddly, MEPAN doesn’t technically fall under the umbrella of NBIA disorders. The few patients to date, including Mike, have disease in the same brain regions and similar symptoms to NBIA, but newer, better MRI technologies have shown us that there is a different type of tissue damage involved, rather than iron accumulation. However, the biochemical pathway involved in MEPAN intersects with NBIA, and the medical management is similar.
Mike is a son, brother, friend, disability awareness consultant, author, playwright, and dancer. Now, he can also say he has MEPAN. He has given an incredible gift to the family of the youngest MEPAN patient—learning of Mike’s sharp mind, wit, and ongoing achievements has created a new world of hope for their young child with this diagnosis. This summer, he will turn 50 years old. We should all raise our glasses to Mike and celebrate his personal accomplishments and his recent, important contributions to science. We can’t wait to see what he does with the next 50 years.
Additional thoughts from Mike Cohn:
 Finding out the true name of what the medical world now calls MEPAN has had a different impact for them than for me, Michael Miller Cohn. I have had to teach the world at large–doctors, nurses, and family friends –who I am and what I can do. Not having a name that people know makes life a very challenging way to live/die.
Finding out the true name of what the medical world now calls MEPAN has had a different impact for them than for me, Michael Miller Cohn. I have had to teach the world at large–doctors, nurses, and family friends –who I am and what I can do. Not having a name that people know makes life a very challenging way to live/die.
I have to still teach even after getting tagged with the name MEPAN. Personally, I still feel alone in this world. No one has come before me. No one can ever share what I see or know what I go through in life day to day. Not having medical pain or organ trouble–just a brain that runs 100,000,000 different ideas.
Some nights I go to sleep wondering, will I wake up? Every day is a TRUE gift. Open eyes, share love and friendship, smell the roses like each day is a new one! Last thing is, I hope some people want to see Mike Cohn the dancer. Yes, dance is a LARGE part of my life. How can a man with a medical tag see life as a dancer? Answer: no labels or tags. Art people do not look for names.
–Mike Cohn, February 18, 2017
You can watch Mike dancing on his Youtube channel:
https://www.youtube.com/channel/UC_wIsg7rFzkYllGtcDeXB4A
Photo courtesy of Tom Wallace at the StarTribute